Drugs across the spectrum 9th edition – Welcome to the world of pharmacology and therapeutics with the esteemed Drugs Across the Spectrum, 9th Edition. This comprehensive resource embarks on an in-depth exploration of the vast spectrum of drugs, their mechanisms of action, therapeutic applications, and potential adverse effects.
Prepare to delve into the intricate world of drug interactions, pharmacokinetics, and pharmacodynamics, unlocking the knowledge essential for safe and effective medication management.
As we journey through this meticulously crafted guide, we will encounter real-world case studies that illuminate the practical application of pharmacological principles. Ethical considerations will be interwoven throughout our discussions, ensuring a well-rounded understanding of the responsibilities and complexities inherent in drug therapy.
Join us on this enlightening odyssey as we navigate the ever-evolving landscape of pharmacology, empowering you with the knowledge to optimize patient outcomes and advance the frontiers of healthcare.
Pharmacological Classification of Drugs
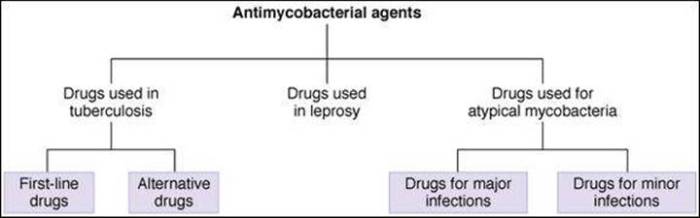
Pharmacological classification of drugs is the process of categorizing drugs based on their pharmacological properties, such as their mechanism of action, chemical structure, or therapeutic effects. This classification system helps researchers, clinicians, and other healthcare professionals understand the different types of drugs available, their potential uses, and their potential risks.
There are several different pharmacological classification systems, each with its own advantages and disadvantages. Some of the most common classification systems include:
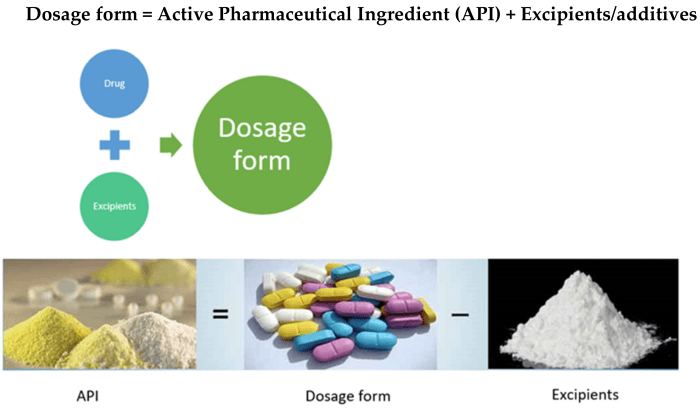
- Anatomical Therapeutic Chemical (ATC) classification system:This system classifies drugs based on their therapeutic use, chemical structure, and pharmacological properties. The ATC system is widely used in Europe and other parts of the world.
- Biopharmaceutical Classification System (BCS):This system classifies drugs based on their solubility and permeability. The BCS is used to predict the bioavailability of drugs and to design drug delivery systems.
- Chemical classification system:This system classifies drugs based on their chemical structure. The chemical classification system is often used in research and development.
- Pharmacodynamic classification system:This system classifies drugs based on their mechanism of action. The pharmacodynamic classification system is often used in clinical practice.
- Therapeutic classification system:This system classifies drugs based on their therapeutic use. The therapeutic classification system is often used by healthcare professionals to select the most appropriate drug for a particular patient.
Each of these classification systems has its own advantages and disadvantages. The ATC system is widely used and provides a comprehensive overview of the different types of drugs available. However, it can be complex and difficult to use. The BCS is a simple and easy-to-use system, but it only classifies drugs based on their solubility and permeability.
The chemical classification system is useful for research and development, but it can be difficult to use for clinical practice. The pharmacodynamic classification system is useful for understanding the mechanism of action of drugs, but it can be difficult to apply in clinical practice.
The therapeutic classification system is easy to use and provides a good overview of the different types of drugs available, but it can be difficult to find the most appropriate drug for a particular patient.
The choice of which classification system to use depends on the specific needs of the user. For example, a researcher may use the chemical classification system to identify new drugs, while a clinician may use the therapeutic classification system to select the most appropriate drug for a patient.
Pharmacokinetics and Pharmacodynamics: Drugs Across The Spectrum 9th Edition
Pharmacokinetics and pharmacodynamics are two important concepts in pharmacology that describe how drugs interact with the body. Pharmacokinetics refers to the processes of absorption, distribution, metabolism, and excretion of drugs, while pharmacodynamics refers to the effects of drugs on the body.
These processes affect the therapeutic effects of drugs. For example, the rate of absorption of a drug will determine how quickly it reaches its target site and how long it will remain in the body. The distribution of a drug will determine which tissues and organs it will reach and how long it will stay in each tissue.
Factors Affecting Pharmacokinetics and Pharmacodynamics
Several factors can alter pharmacokinetics and pharmacodynamics, including:
- Age
- Weight
- Gender
- Genetics
- Health conditions
- Drug interactions
It is important to consider these factors when prescribing drugs to ensure that the patient receives the correct dose and that the drug is effective and safe.
Drug Interactions
Drug interactions occur when two or more drugs are taken together and produce an effect that is different from the effect of either drug taken alone. Drug interactions can be beneficial, harmful, or have no effect at all. The clinical significance of a drug interaction depends on the nature of the interaction and the drugs involved.
Types of Drug Interactions
There are many different types of drug interactions. Some of the most common types include:
- Pharmacokinetic interactionsoccur when one drug affects the absorption, distribution, metabolism, or excretion of another drug. For example, one drug may increase the absorption of another drug, leading to higher blood levels of the second drug.
- Pharmacodynamic interactionsoccur when one drug affects the effect of another drug at the receptor level.
For example, one drug may block the receptor for another drug, preventing the second drug from having its desired effect.
- Drug-herb interactionsoccur when a drug interacts with a herb or other natural product. For example, St. John’s wort can interact with many different drugs, including antidepressants, birth control pills, and blood thinners.
Examples of Common Drug Interactions
Some common examples of drug interactions include:
- Warfarin(a blood thinner) can interact with many different drugs, including aspirin, ibuprofen, and antibiotics. These interactions can increase the risk of bleeding.
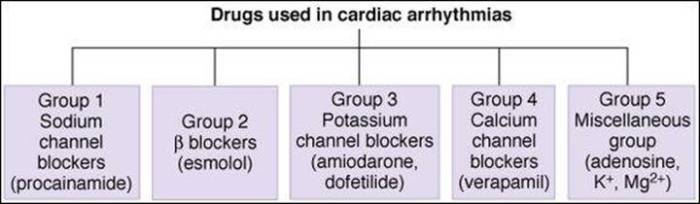
- Metoprolol(a beta-blocker) can interact with calcium channel blockers, such as diltiazem and verapamil. These interactions can lead to low blood pressure and bradycardia.
- Grapefruit juicecan interact with many different drugs, including statins, calcium channel blockers, and antihistamines. These interactions can increase the blood levels of the drugs, leading to an increased risk of side effects.
Clinical Significance of Drug Interactions
Drug interactions can have a significant impact on patient care. They can lead to:
- Increased risk of side effects
- Decreased effectiveness of drugs
- Drug toxicity
- Death
It is important for healthcare professionals to be aware of potential drug interactions and to take steps to prevent them. This can be done by:
- Asking patients about all of the drugs they are taking, including over-the-counter drugs and herbal supplements.
- Checking for potential drug interactions before prescribing a new drug.
- Monitoring patients for signs and symptoms of drug interactions.
- Adjusting the dose of a drug or discontinuing a drug if an interaction is suspected.
Adverse Drug Reactions
An adverse drug reaction (ADR) is any unwanted or harmful effect that occurs as a result of taking a medication. ADRs can range from mild and temporary to severe and life-threatening.
ADRs are classified into different types based on their severity and the way they occur.
Types of ADRs
- Mild ADRsare common and usually do not require medical treatment. Examples include nausea, vomiting, and diarrhea.
- Moderate ADRsare more severe and may require medical treatment. Examples include rash, itching, and swelling.
- Severe ADRsare rare but can be life-threatening. Examples include anaphylaxis, Stevens-Johnson syndrome, and toxic epidermal necrolysis.
- Delayed ADRsoccur after the medication has been stopped. Examples include liver damage, kidney damage, and cancer.
The risk of ADRs is increased by several factors, including:
Factors that Increase the Risk of ADRs
- Age: Older adults are more likely to experience ADRs.
- Underlying medical conditions: People with certain medical conditions are more likely to experience ADRs.
- Drug interactions: Taking multiple medications can increase the risk of ADRs.
- Dosage: Taking too much of a medication can increase the risk of ADRs.
Drug Abuse and Addiction
Drug abuse refers to the misuse of drugs, including prescription medications, illicit substances, and over-the-counter drugs, in a manner that deviates from their intended purpose. Addiction, also known as substance use disorder, is a chronic, relapsing brain disease characterized by compulsive drug-seeking and use despite negative consequences.
Signs and Symptoms of Drug Abuse and Addiction
The signs and symptoms of drug abuse and addiction can vary depending on the type of drug being used. However, some common indicators include:
- Changes in behavior, such as increased secrecy, irritability, or isolation
- Physical changes, such as weight loss, changes in sleep patterns, or dilated pupils
- Problems at work, school, or in relationships
- Financial difficulties
- Legal problems
Treatment for Drug Abuse and Addiction
Treatment for drug abuse and addiction typically involves a combination of approaches, including:
- Behavioral therapy:This type of therapy helps individuals learn coping mechanisms, change their behavior, and develop relapse prevention strategies.
- Medication:Medications can be used to reduce cravings, block the effects of drugs, or treat co-occurring mental health conditions.
- Support groups:Support groups, such as Alcoholics Anonymous or Narcotics Anonymous, provide a supportive environment for individuals in recovery.
- Inpatient treatment:Inpatient treatment programs provide a structured and supervised environment for individuals to focus on their recovery.
- Outpatient treatment:Outpatient treatment programs allow individuals to continue with their daily lives while receiving treatment.
Drug Regulation
Drug regulation plays a crucial role in ensuring the safety and efficacy of drugs before they are made available to the public. Various regulatory agencies oversee the development and marketing of drugs to safeguard public health.
The drug development process involves rigorous testing and evaluation to assess a drug’s safety, effectiveness, and potential risks. Clinical trials are conducted in phases to gather data on the drug’s performance and identify any adverse effects.
Regulatory Agencies
- Food and Drug Administration (FDA): The primary regulatory agency in the United States responsible for overseeing the development, approval, and marketing of drugs, biologics, and medical devices.
- European Medicines Agency (EMA): The central authority for the evaluation and supervision of medicinal products in the European Union.
- World Health Organization (WHO): Provides global leadership and guidance on drug regulation and safety through its various initiatives and programs.
Clinical Trial Phases
- Phase I: Initial safety and dosage studies conducted on a small group of healthy volunteers.
- Phase II: Expanded studies to assess efficacy and safety in patients with the target condition.
- Phase III: Large-scale clinical trials to confirm efficacy and safety in a broader patient population.
- Phase IV: Post-marketing surveillance studies to monitor long-term safety and effectiveness in real-world settings.
Drug Approval Process
The drug approval process involves a thorough review of the data collected during clinical trials and other supporting information. Regulatory agencies evaluate the drug’s benefits and risks to determine its suitability for public use.
- Submission of Application: Pharmaceutical companies submit a New Drug Application (NDA) or Biologics License Application (BLA) to the regulatory agency.
- Review and Evaluation: The agency conducts a comprehensive review of the application, including data on safety, efficacy, and manufacturing processes.
- Approval or Rejection: Based on the review, the agency grants approval or issues a rejection letter detailing the reasons for the decision.
- Post-Approval Monitoring: Once approved, drugs are subject to ongoing monitoring and surveillance to ensure continued safety and effectiveness.
Special Populations
Drug therapy in different populations, such as children, pregnant women, and the elderly, requires special considerations. These populations have unique physiological and developmental characteristics that can affect drug absorption, distribution, metabolism, and excretion.
Adjusting drug dosage in these populations is crucial to ensure efficacy and minimize adverse effects. Factors to consider include age, weight, renal function, hepatic function, and co-existing medical conditions.
Children
Children’s bodies are still developing, and their drug metabolism and excretion pathways may not be fully mature. This can lead to differences in drug absorption, distribution, and elimination compared to adults.
- Drug dosages for children are typically calculated based on body weight or body surface area.
- Certain drugs may require more frequent dosing in children due to their faster metabolism.
- Special formulations, such as liquid suspensions or chewable tablets, may be necessary for children who have difficulty swallowing pills.
Pregnant Women
During pregnancy, physiological changes occur that can affect drug absorption, distribution, metabolism, and excretion. Additionally, certain drugs can cross the placenta and reach the fetus, potentially causing adverse effects.
- Pregnant women should only take medications that are essential and have been deemed safe for use during pregnancy.
- The use of certain drugs, such as teratogens, is contraindicated during pregnancy due to the risk of birth defects.
- Drug dosages may need to be adjusted throughout pregnancy to account for changes in maternal physiology.
Elderly
As people age, their bodies undergo physiological changes that can affect drug absorption, distribution, metabolism, and excretion. Additionally, elderly patients are more likely to have multiple co-existing medical conditions and take multiple medications, increasing the risk of drug interactions.
- Drug dosages for elderly patients may need to be reduced due to decreased renal function and hepatic metabolism.
- Elderly patients may be more sensitive to the adverse effects of certain drugs.
- Polypharmacy, or the use of multiple medications, can increase the risk of drug interactions and adverse effects in elderly patients.
Case Studies
Case studies provide valuable insights into the complexities of drug-related problems, highlighting the interplay of individual, environmental, and societal factors that can contribute to adverse outcomes.
By examining real-world scenarios, we can gain a deeper understanding of the challenges faced by patients and healthcare professionals, and identify strategies for prevention and intervention.
Factors Contributing to Drug-Related Problems
- Patient factors:Age, genetics, comorbidities, lifestyle choices, and mental health status can influence drug response and susceptibility to adverse events.
- Drug factors:Drug interactions, adverse effects, and misuse or abuse can lead to serious health consequences.
- Healthcare provider factors:Prescribing errors, inadequate patient education, and lack of follow-up can contribute to drug-related problems.
- Societal factors:Socioeconomic status, access to healthcare, and cultural beliefs can impact drug use and outcomes.
Case Example: Polypharmacy in the Elderly
An 85-year-old patient with multiple chronic conditions was taking 15 different medications. Due to age-related changes in drug metabolism and excretion, she experienced several adverse drug reactions, including confusion, dizziness, and falls.
A comprehensive medication review revealed that many of the medications were unnecessary or could be replaced with safer alternatives. By reducing the number of medications and optimizing dosing, the patient’s symptoms resolved, and her quality of life improved.
Case Example: Drug Misuse in Adolescents
A 16-year-old high school student was admitted to the emergency department with alcohol poisoning. She had been drinking heavily with friends at a party and had lost consciousness.
Social work assessment revealed that she was experiencing stress and anxiety related to academic pressure and family problems. She had turned to alcohol as a coping mechanism.
Treatment involved detoxification, counseling, and support group participation. The student developed healthier coping strategies and was able to reduce her alcohol use.
Conclusion
Case studies illustrate the complexities of drug-related problems and emphasize the importance of a multidisciplinary approach to prevention and management.
By understanding the factors that contribute to adverse outcomes, healthcare professionals can work with patients to develop individualized treatment plans that promote safe and effective drug use.
Ethical Considerations
Drug therapy presents ethical considerations that healthcare professionals must navigate to ensure the responsible and appropriate use of medications. These considerations involve balancing the potential benefits and risks of drug therapy, respecting patient autonomy, and ensuring equitable access to essential medicines.
Ethical principles provide a framework for guiding drug therapy. These principles include:
- Beneficence: The obligation to act in the best interests of the patient, prioritizing their well-being and maximizing potential benefits.
- Non-maleficence: The duty to avoid causing harm, minimizing risks and adverse effects associated with drug therapy.
- Autonomy: Respecting the patient’s right to make informed decisions about their healthcare, including the choice to accept or refuse treatment.
- Justice: Ensuring fair and equitable distribution of healthcare resources, including access to essential medicines for all individuals.
Ethical Dilemmas in Drug Therapy, Drugs across the spectrum 9th edition
Ethical dilemmas arise in drug therapy when these principles conflict or when the best course of action is unclear. Examples include:
- Informed consent: Balancing the patient’s right to make informed decisions with the need for timely and effective treatment in emergency situations.
- Confidentiality: Maintaining patient privacy while reporting adverse drug reactions or potential drug interactions to regulatory authorities.
- End-of-life care: Determining the appropriate use of medications for symptom management and pain relief in terminally ill patients, considering their wishes and quality of life.
- Placebo effects: Deciding whether to use placebos in clinical trials or as a therapeutic intervention, considering the potential benefits and risks of deception.
- Drug pricing: Balancing the need for innovation and research with ensuring affordability and access to essential medicines for all.
Answers to Common Questions
What are the major drug classifications?
Drugs are classified based on their pharmacological properties, therapeutic uses, chemical structure, and mechanism of action. Common classifications include antidepressants, antibiotics, antipsychotics, cardiovascular drugs, and analgesics.
How do drugs interact with the body?
Drugs interact with the body through various mechanisms, including binding to receptors, inhibiting enzymes, or altering ion channels. These interactions can lead to therapeutic effects or adverse reactions.
What factors can affect drug metabolism?
Drug metabolism can be influenced by factors such as age, genetics, liver function, and concomitant medications. Understanding these factors is crucial for optimizing drug therapy.
What are the common types of adverse drug reactions?
Adverse drug reactions can range from mild (e.g., nausea) to severe (e.g., anaphylaxis). Common types include allergic reactions, gastrointestinal disturbances, and hepatotoxicity.
How is drug abuse defined?
Drug abuse refers to the excessive or improper use of drugs, leading to harmful consequences for the individual or society. It can involve illegal substances or prescription drugs used in a non-prescribed manner.
